Table of Contents
One day, out of the blue, I ( Jane May Graves, CEO of Luxe Beauty) received an email from Optometrist Dr. Michele Pendrak thanking me for not using Retinol in my products. I asked her for more details and was shocked by what she shared. I wanted to share it with you.
Before Speaking with Dr. Pendrak, I knew Retinol could make your skin more sensitive to other products.
For example, there are recommendations to limit face scrubs, vitamin C, toners, astringents, and other facial treatments while using Retinol.
Another well-known aspect of Retinol and retinoids is that they can make your skin more sensitive to sunlight. Experts advise using them at night and wearing strong sunscreen daily because your skin is more likely to burn.
It's also possible that this increased sensitivity may open you up to a greater skin cancer risk. Animal studies have found that retinyl palmitate and retinoic acid, in particular, can increase tumor growth on exposure to synthetic sunlight.
We must remember that our skin is our shield and protection from damage and all oxidative stress. I don't know about you, but I never want to make my largest organ ( skin) more sensitive. My philosophy is to support all organs with nourishing ingredients.
Below is what Dr. Michele Pendrak shared, observed, and learned about Retinol by seeing hundreds of patients, even patients in their 20s:
"According to research published on PubMed, since retinol can damage the eyes, you should be cautious of any serum or cream containing retinol as an ingredient.¹
Unfortunately, retinol can be a foe to your eyes.
At this point, my patients usually start shooting eye daggers at me. But before you break out your pitchforks, allow me to explain! Today, there are healthier, clean alternatives to help you achieve that youthful glow than ever before.
What are retinoids?
So, first, let’s talk about what retinoids are. Retinoids are a group of compounds that are Vitamin A derivatives.
There are 6 types of retinoids:
1)retinol (the natural form of Vitamin A)
2)tretinoin (synthetic, prescription only, and also branded as Retin-A cream)
3)Adapalene (branded as Differin gel)
4)tazarotene
5)alitretinoin
6)bexarotene.
All of the above have become popular in the skin care industry mainly because, when used topically, they increase cell turnover and can increase collagen and elastin.
Increased cell turnover has many benefits, including unclogged pores and anti-aging effects.
The most commonly used retinoid creams for skin care are retinol and tretinoin. Retinol has to be converted by our skin enzymes into retinoic acid, which slows down its effects. Therefore it can take about six months of using it to notice retinol’s cumulative benefits, but this also makes it a gentler product with fewer side effects.
Therefore, Tretinoin does not need to be converted and acts faster, with results in 6 to 8 weeks. For this reason, it is a more vital medication. The general rule with medications is stronger = greater side effects; the same is true here.
Why are retinoids bad for my eyes?
What are the side effects of retinol? 2 words:
1) drying
2) scarring.
Even if you are not using a retinol eye cream or feel that you are keeping it away from your eyes, you never know how much of that cream can migrate toward your eyes ( yes, it does migrate!). And this brings several concerns.
We have three layers to our tear film. The top layer is oil, which acts as a moisture seal to prevent evaporation. We get this oil from the approximately 25 meibomian glands running vertically along our upper and lower eyelids. 86% of dry eye falls under the category of evaporative dry eye ¹ - meaning we don’t have enough oil. It is currently estimated that approximately 49 million Americans have dry eye - compare this to the fact that 3 million have glaucoma².
Many patients with evaporative dry eyes have fluctuating filmy, hazy, and blurry vision.
Dry eye symptoms can also include red, burning, scratchy, stinging, and watery eyes (yes, I know that last one is counterintuitive!). If left untreated, it can even lead to corneal scarring and nerve damage.
As time passes, we realize how susceptible the oil glands are to damage from specific products and medications.
And - you guessed it - the retinoids are at the top of the list of offenders that are known to cause damage to the meibomian glands.
Retinoids work for acne by shrinking oil glands but can also decrease oil production everywhere. That includes the delicate oil glands in our eyelids.
Generally, the meibomian glands follow the rule "if you don't use it, you lose it"- meaning if our bodies get signals not to use the glands, they shrink and atrophy or drop out.
This atrophy is darn near impossible to reverse. Studies have found retinoic acid "alters meibomian gland epithelial cell gene expression, reduces the activity of cell survival mediators, inhibits proliferation, and induces meibocyte cell death." ³ In other words - it kills our meibomian glands.
Over the years, I have consistently seen patients, even as young as 25, come into my office with atrophied meibomian glands with a history of retinoid use.
Once you've seen a parade of meibomian glands completely atrophied by-products such as retinoids day in and day out, you can't go back!
Patient Example:
Recently, I saw a 61-year-old with a history of retinol cream use whose dry eye I finally have under control after four years of treatment (we got interrupted by the pandemic). When I started treating her in 2018, she always returned for dry eye follow-ups, showing little to no improvement despite aggressive treatments. Finally, I noticed her gorgeous skin and asked about her skincare regimen. She was using retinol creams. Around this time, we also obtained a meibographer - a camera that does infrared imaging of the meibomian or oil glands in the eyelids. And suddenly, it all became clear.
Her glands were partially atrophied, possibly from years of retinol use, so she wasn’t giving me much to work with. This scarring is widespread with retinoid use and complicates treating the glands. I am fortunate to have an in-house surgeon who performs meibomian gland probing because less than 3% of eye doctors in the country do this⁴. It is one of the few documented procedures to help regenerate atrophied glands. The images of her meibomian glands are below.
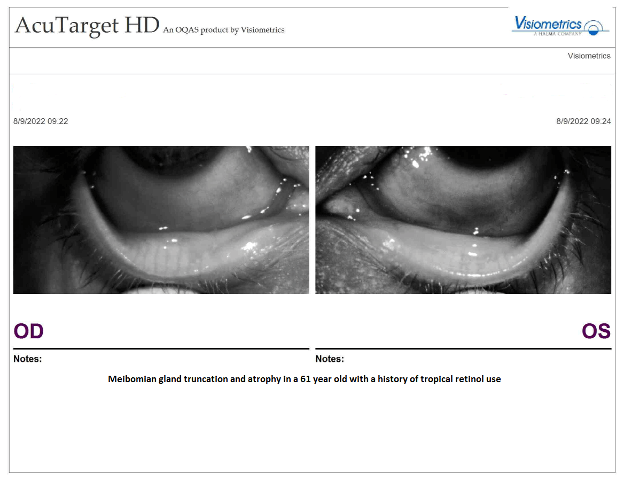
The picture is meibography, or infrared imaging of his meibomian glands. You’ll notice that her “OD” which is her right, has worse shortening of the white columns (the meibomian glands) on the right side of the picture. Her “OS” or left eye, has a more significant shortening throughout the length of the lid.
Also, despite our best efforts, if she was going home and putting a cream on or around her eyes that was drying her out, she was undoing all of our hard work!
Retinol is also stored in the lacrimal gland, which secretes the middle watery layer of our tear film. Retinol has been isolated in rabbit and human tears ⁵. It, therefore, should come as no surprise that we have seen cases of lacrimal gland atrophy ⁶ in people with a history of retinoid use.
Learning from my experience:
After this patient, I added a section to my Dry Eye Intake Questionnaire about anti-aging products and procedures, specifically asking about upfront retinol use. This patient taught me I needed to ask about retinol use before starting treatment.
I needed to allow my patients to understand where their dry eye may be coming from, counsel them on healthy alternatives, and understand what treatment challenges we may face.
My clinic offers powerful light-based treatments, quickly becoming the gold standard for treating dry eye. These treatments, such as Low-Level Light Therapy and Intense Pulsed Light Therapy, also offer excellent aesthetic benefits. Gone are the days when we had to choose between treating our skin or caring for our eyes.
So is a skin cream worth all of that? And if we can’t use retinol, what can we do instead?
If retinol was the only anti-acne or anti-aging treatment out there, I could see where someone feeling invincible would occasionally take their chances.
However, there are so many other alternatives. Gone are the days when we had to choose between treating our skin or caring for our eyes.
Thankfully, it is easier than ever to find clean products that are good for our skin and eyes. I love how Companies like Luxe Beauty make safe products like their luxurious night cream and anti-aging serum with hyaluronic acid and peptides.
Rosehip Oil is a natural retinol because it contains natural retinoic acid. The kind of vitamin A found in rosehip oil is more beneficial than retinol. This is because your skin will recognize it immediately, so it won't need time to convert it.
I love and recommend Luxe Beauty's antioxidant serum because one of the main ingredients is rosehip oil. I tell my patients to research all their skincare ingredients to ensure no retinol in their products. Thankfully, nature has provided us with safe and natural retinol by creating rosehip oil.
It makes me so happy to see so many people (like you!) pushing back, researching, and seeking healthy alternatives to retinol. " Dr. Michele Pendrak
References
1- https://pubmed.ncbi.nlm.nih.gov/22378109/
2- USA General Population 2018 Cross Sectional Study and Census.gov Population Clock
3- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3694789/
5- https://pubmed.ncbi.nlm.nih.gov/2950849/
6- https://pubmed.ncbi.nlm.nih.gov/33470346/
Dr. Michele Pendrak is an optometrist who specializes in the ocular surface disease. She is currently at Siepser Eyecare in Wayne, PA, where she recently oversaw the clinic’s opening of the area’s first and only Dry Eye Center of Excellence. Her specialty has led her to have an interest in clean makeup and personal care products, a topic she often lectures on.
Disclaimer: Content in this blog and on our website is not a substitute for professional medical or healthcare advice, diagnosis, treatment, dietary, or safety advice and may not be used for such purposes. Always seek the advice of your physician or other qualified experts with any questions you may have regarding a medical question, condition, or safety concern. Reliance on information presented on this site is at your own risk.